There are only a few things in this world that can make you more uncomfortable than having *that area* begging for a good scratch fest. There are a lot of dos and don'ts when it comes to cleaning, of course, but what’s the protocol when vaginal itching is keeping you up at night?
Let's get clear on the subject at hand here: When women talk about vaginal itching, many are actually referring to itching in the vulva, the outer part of the female genitalia, says Mary Jane Minkin, MD, an ob-gyn and a clinical professor at Yale University School of Medicine. “True vaginal itching is less common,” she adds.
You should also know that itching in the nether regions is very common, and there are many reasons that could explain it, says Alyssa Dweck, MD, an ob-gyn in Westchester County, New York. Really, having an itchy vagina is one of the main reasons people go see their gynecologist, notes Katharine O'Connell White, MD, an ob-gyn and associate professor in the department of obstetrics and gynecology at Boston University.
Anything from an infection (like a yeast infection or bacteria vaginosis) to skin conditions like eczema, psoriasis, or pubic lice could be to blame here, says Leah S. Millheiser, MD, a clinical professor in the department of obstetrics and gynecology at Stanford Medicine.
Meet the experts: Alyssa Dweck, MD, is an ob-gyn in Westchester County, New York. Katharine O'Connell White, MD, is an ob-gyn and associate professor in the department of obstetrics and gynecology at Boston University. Leah S. Millheiser, MD, is a clinical professor in the department of obstetrics and gynecology at Stanford Medicine.
But itching can also have causes unrelated to any underlying medical condition. Your vagina could just be irritated by detergent residue on your underwear, menstrual pads, or a lubricant or spermicide, says Dr. White. Or your clothes could just be too tight, Dr. Millheiser adds. If the itchiness continues after seconds or a few minutes, there’s a good chance you need to get your itch down there checked out by a doc, says Kimberly Langdon, MD, a retired ob-gyn.
Want to know what you may be dealing with? Here are all the reasons you’re urging to scratch your nether regions RN—and, of course, how to treat it.
1. You have bacterial vaginosis (BV).
Bacterial vaginosis is a pretty common condition caused by bacterial overgrowth and a pH imbalance in the vagina. Though it can affect all women, higher rates of BV are particularly prevalent among Black women. Experts don't really know why yet, says Carroll Medeiros, MD, an ob-gyn with Partners in Obstetrics and Gynecology. It may be related to genetic predisposition, per one 2016 study in the American Journal of Reproductive Immunology.
But itching actually isn’t the primary symptom of BV—the hallmarks are typically a loose discharge, strong odor, and general irritation (though it definitely can make you itchy too), says Dr. Minkin.
To treat it, you can try an OTC medication like RepHresh to up the acidity of your vagina, according to Dr. Minkin. Sounds counterintuitive, but acidity in the vagina is actually a good thing since it kills off bad bacteria, she explains. If that doesn’t work, your doc might prescribe antibiotics.
2. You have eczema or psoriasis.
"Skin conditions like eczema and psoriasis can occur due to an allergy or autoimmune issue,” says Natasha Chinn, MD, an ob-gyn with Brescia and Migliaccio Women’s Health in New Jersey. Eczema often appears in the crevices of arms, folds, the groin area, and on the labia, she explains. Psoriasis can also present on the skin around the vagina, she adds.
Most people with eczema and psoriasis are well-versed in the appearance (and treatment) of these red, patchy rashes. But if you’ve never had these symptoms before, make an appointment with your doctor. Both conditions can be managed if they’re flaring up, and Dr. Chinn says that psoriasis sometimes warrants a prescription for an oral pill or a topical cream.
3. You have contact dermatitis.
Ever try a new body cream and wind up with dried out, flaky skin or a full-blown rash a few days later? Well, the same thing can happen to the skin around the vagina. “Soaps, detergents, and bubble baths, a new kind of underwear—really any new products at all that come in contact with your vagina [can cause itching],” explains Dr. Minkin.
If your vagina feels itchy and irritated, but you don’t have any other symptoms, it’s worth thinking about whether you’ve recently started using any new products. Pads and tampons, condoms, and lubricants, shaving products, and even toilet paper can all be to blame (basically anything with added perfumes or chemicals, so stick with hypoallergenic stuff if you’re sensitive).
In the meantime, stop using whatever you think is bugging you, treat the itch with an Epsom salt bath or an OTC hydrocortisone cream applied externally, and wait a few days to see if the itch resolves. If not, go see your doctor.
4. You have a yeast infection.
Vaginal yeast infections, which occur when there is an overgrowth of the fungus Candida, are probably the first thing people think of when they feel that telltale itching down there. “A cottage cheese-like discharge, redness around the labia and vulva, and itching are all classic signs of a yeast infection,” Dr. Minkin says.
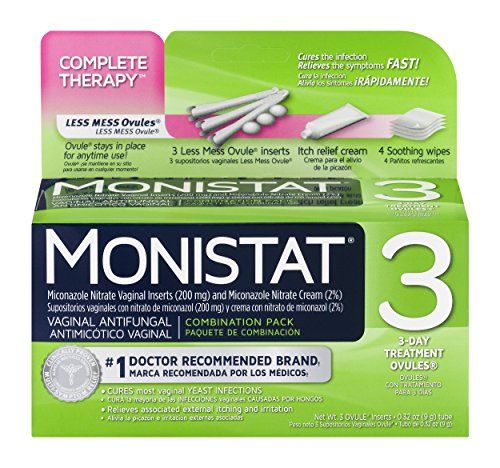
But she also notes that only about one-third of women who experience itching and irritation truly do have a yeast infection. The easiest way to tell which category you fall into is to use an OTC treatment like Monistat. Dr. Minkin says that if you really do have a yeast infection, it should do the trick; if it doesn’t, check in with your provider.
5. You have a sexually transmitted infection (STIs).
Itching isn't really a classic symptom of most STIs, though it can sometimes be a first sign that something is up, says Dr. Minkin. From there, symptoms may progress to burning, painful urination, smelly discharge, sores on your genitals, or painful intercourse, at which point you should definitely head to your ob-gyn for a vaginal culture.
The STIs below are most commonly associated with vaginal itchiness, among other symptoms. Here's what to look out for.
- Genital warts. Genital wars are small, flat, flesh-colored bumps or tiny, cauliflower-like bumps that appear on the skin, resulting from exposure to the human papilloma virus. “This type of STI can shift the pH in the vagina, which then causes dryness and itching," says Dr. Chinn.
- Herpes. Genital herpes causes clusters of red, blistery bumps on the vulva, which come and go as outbreaks. You may experience itching in the areas the sores appear in even before they show up.
- Chlamydia. Chlamydial infections will usually not show any symptoms. But in rarer cases, chlamydia can lead to itching and irritation of the genital area, discomfort when urinating, and an unusual discharge.
- Gonorrhea. Gonorrhea is an infection of the genitals, rectum, or throat. Symptoms can include itching, increased vaginal discharge, and a painful or burning sensation when peeing.
- Trichomoniasis. This STI is caused by an infection from a protozoan parasite called Trichomonas vaginalis. Only about 30 percent of people with the infection show symptoms, but they can include itching, burning, redness, or soreness of the genitals.
FYI, there are many ways to treat STIs, and Dr. Minkin suggests seeking the advice of a trusted medical professional if you have one. For some, you need to take antibiotics, like cefatriaxone for gonorrhea, or azithromycin and tetracycline for chlamydia. Herpes, on the other hand, can be treated with valacyclovir, she adds.
Some are more dangerous, like syphilis, which you need to see a doctor to be diagnosed, then you can receive penicillin to treat it. And remember: The best ways to avoid getting HPV are to get vaccinated and make sure your partner does the same. (It also goes without saying that wearing condoms can help prevent STIs from spreading.)
6. You have pubic lice.
No one wants to think about bugs crawling around on any part of their body, but especially not down there. Unfortunately, that’s exactly what pubic lice (a.k.a. crabs) is: an easily transmittable infestation of little bugs in your genital area that makes you itch like crazy.
There are two reasons for the itching, says Dr. Chinn: bites from the crabs and the eggs (nits) they lay on your skin, both of which cause irritation.
Now for the really bad news: Having sex isn’t even the only way to get pubic lice. “They’re passed from skin to skin,” says Dr. Chinn. “[For example], you go to a dirty hotel and there are nits or lice in the sheets you slept on, and then you go home to your partner and have sex. Or maybe you loan your sister your pants and [she] had them, then you wear the pants and the crabs crawl into the vaginal area."
Though treatable with an OTC medication like permethrin cream (just like head lice), the morals of the story here are as follows: practice safe sex, read hotel ratings carefully, and maybe don’t let anyone borrow your pants (and vice versa).
7. You have lichen sclerosus.
Another dermatology issue, lichen sclerosus is a patchy white rash that causes intense itching and often pops up in your genital area (though it can appear on other parts of the body too). It can be treated with a prescription-strength topical steroid, but Dr. Minkin says a lichen sclerosus rash can often mimic vulvar cancer, so its appearance may complicate things a little.
“In young women, it’s more likely to be lichen sclerosus than cancer, but I’ll often bring patients back in a few weeks to see how it’s looking, especially if they are older,” says Dr. Minkin. “We want to make sure we’re not missing cancer, so if it hasn’t cleared up with steroids, I may do a biopsy to scan it.”
8. You're going through hormonal changes or perimenopause.
When your hormones fluctuate during your menstrual cycle, you might end up with drier vaginal tissue than normal, which can cause itching. But Dr. Minkin points out that perimenopause (that time period before you actually start menopause) is a more common time for vaginal dryness and itching, thanks to the drop in estrogen.
An OTC moisturizer like Replens can usually provide relief from internal itching for about three days, Dr. Minkin says, and your provider can give you a prescription estrogen cream for any external itching. (And if any vaginal dryness is impacting your sex life, just know adding lube down there will do the trick.)
And yup, it’s possible for pregnancy to cause vaginal itchiness and dryness too. How so? The common hormonal changes during pregnancy can disrupt the vaginal biome’s typical pH, says Dr. Dweck. This is what makes yeast infections pretty darn regular during pregnancy, explains Dr. Dweck.
9. You have a urinary tract infection (UTI).
A urinary tract infection is a bacterial infection that crops up anywhere in your urinary tract (read: kidneys, urethra, ureters, and bladder), and will commonly cause pelvic pain, a strong urge to pee, a burning sensation while urinating, and cloudy or foul-smelling urine.
But Dr. Minkin confirms that it can also cause itching in the form of a tingling, irritated sensation, especially if the infection is located near your urethra. You need to snag an appointment with your doctor ASAP and get a urinalysis to check for the presence of bacteria (which an antibiotic can clear up).
10. Your beauty treatments are causing irritation.
In the past few decades, women have grown more preoccupied with the appearance of their vulvas, says Dr. Minkin—something she attributes to the trend of having less hair down there. That means many women have also tried out some pretty unconventional beauty treatments, like activated charcoal vulva masks (basically a facial for your vagina) and vaginal steaming.
These are a no-no, not only because they’re totally unnecessary, but also because they can cause itching and irritation, Dr. Minkin says. “The vulva tissue is the most sensitive, delicate tissue in the body,” she adds. “Treat it with respect and a gentle hand. The less stuff you do to it, the better.” Noted!
11. You have a tanning bed burn.
Reminder: You should *not* be using tanning beds. Not only can they up your risk of developing skin cancer, but tanning in the nude can give you a burn on the skin around the vagina. “Redness and peeling of the skin causes itching—that's what tends to happen when women go to a tanning bed,” says Dr. Chinn.
So yeah, just don't do this in the first place, please. But if you do somehow end up with a burn downstairs, Dr. Chinn says you can mix a little aloe vera with coconut oil or tea tree oil and apply it topically (it’s perfectly safe for the vaginal area).
12. You have a razor burn down there.
Your bikini area is just as sensitive—if not more so—to razor burns and irritation from shaving or waxing your hair. "When we wax or shave anywhere on the body, we disrupt the skin's integrity,” says Dr. Chinn. “Redness, itching, and burning can occur if you're sensitive to it.”
If you have curly or coarser hair down there, you're more at risk for razor bumps and ingrowns, since it's easier for this kind of hair to become caught under the skin's surface. Not having access to good quality depilatories and shavers can also put you at a greater risk of developing itching from hair removal irritation, Dr. Medeiros adds.
Dr. Chinn recommends applying hypoallergenic creams or lotions to protect the skin, as well as keeping it dry and clean. If it’s becoming an ongoing problem for you, you may have to stop waxing, wax less frequently, or change up your shaving products to something gentler on your skin, she adds.
13. You have vulvar cancer.
Vulvar cancer is a rarer cancer that's typically diagnosed in older women, says Dr. Medeiros. It's caused by an abnormal growth of cancerous cells in the vulva. Most women who get it don't really noticed they have it until a doctor sees an irregularity, like a lesion, on their skin, she explains.
Itching that's associated with this condition tends to be localized to the area where the cancer is. "The kind of itching you have from a vulvar malignancy tends to turn into pain really quickly; as the cancer grows superficially and deeply, it pinches upon nerves and causes pain," says Dr. Medeiros.
This is pretty rare. And though vulvar cancer may cause itching, you'll probably experience other symptoms like skin changes too. If you're concerned, it's best to consult your doctor, who can take a closer look.
14. You have lichen planus.
Lichen planus is "a condition that causes swelling and irritation that happens when your immune system attacks cells of the skin or mucous membranes (like the vagina)," Dr. White explains. While medical professionals still don't know why it happens, the good news is that it it isn't contagious.
Although anyone can develop it, but people in their 40s and 50s are most often affected. Still, it's pretty rare—it impacts just one to two percent of the world's population, Dr. White says.
Itching is a very common symptom, especially when it occurs in the vaginal area, says Dr. Medeiros. People with lichen planus may also notice painful sores and blisters.
A topical low-potency or high-potency steroid is the mainstay treatment for lichen planus, but Dr. Medeiros recommends consulting a dermatologist to figure out the best treatment.
So, why does my vagina itch more at night?
If the temptation to scratch becomes even more unbearable at night, you're not alone. Because you aren't distracted by work, phone calls, and all that other daytime stuff, you can become hyper-aware of an itchy vagina (or any part of the body) at night, says Dr. Medeiros.
Is it possible to have itching without discharge?
Vaginal itching is typically accompanied by symptoms like unusual discharge, a foul odor, redness, or abnormal bleeding, says Dr. Dweck.
That said, it’s quite possible that you’re experiencing vaginal itching without noticing any discharge. “While discharge and itching often go hand in hand, it's totally possible to have one without the other,” Dr. White says.
In short, don’t worry if you feel like your symptoms are atypical. Consult your doctor to talk through what you’re experiencing before stressing out. (Odds are it’s nothing serious!)
What can I use to stop the itching?
First things first, always consult your gynecologist before trying any kind of DIY treatment. Once you’re on the same page as your gyno, there are ways to reduce your itching symptoms at home.
If you have a yeast infection, you can try a mixture of yogurt and honey, which one 2015 study shows could be just as effective as an antifungal cream at relieving some symptoms. That said, OTC creams like Monistat can get rid of the infection in most cases, Dr. Dweck says.
If you're dealing with a rash caused by an external irritant (hi, laundry detergent and pesky thongs), an OTC hydrocortisone cream can be helpful, Dr. Dweck says. You’d only need prescription-strength cortisone if your symptoms are severe.
Cold compresses or ice packs to the vulva can ease the itching too, Dr. Dweck says. But try not to put ice directly on your skin and make sure you place a cloth in-between!
You can also try taking oatmeal baths or baking soda soaks for 10 to 15 minutes at a time, a few times per day, Dr. White says. Just add four to five tablespoons of baking soda to lukewarm water and relax.
When do you need to see a doctor?
The following symptoms are indicators that you need to check in with your gyno, according to Drs. Langdon and Millhesier.
- An abnormal vaginal discharge associated with itching
- Any sort of rash or lumps
- Burning or pain
- Changes in the appearance of the vulvar skin associated with itching;
- Excoriation of the labia minora, perineum
- Foul-smelling discharge
- Lesions of the vulva that cause itching
- Moderate to severe persistent itching
- Swelling of the labia minora
- White cottage cheese discharge
If vaginal itchiness does not go away with washing, drying, and a change of panties, Dr. Langdon says you should see your doctor.
Can you prevent vaginal itching?
Yep, vaginal itching is preventable. (Though not always!) The key is to follow a few different hygiene tips that’ll ensure you’re not messing with your vagina’s pH.
- Dr. Medeiros recommends staying away from harsh cleansers. Instead, go for products like a Dove fragrance-free wash. Her rule of thumb is if you wouldn't put it on your face, don't put it near your vagina. (You also only need your fingers, soap, and water—no washcloths or loofahs, Dr. White adds.)
- When you’re out of the shower, be sure to pat your vulva dry—don’t rub, Dr. White says. And make sure you buy soft, white, unscented toilet paper. You don’t need to use any powders or sprays on your vulva either, as it’s totally normal for your vagina to have its own natural scent, Dr. White says.
- If you find that you’re sensitive to menstrual hygiene products, try swapping out your usual ones for organic cotton tampons and pads, or a medical-grade silicone menstrual cup, Dr. Dweck says. And yup, your undies can cause vaginal itchiness too. Opt for 100 percent cotton panties, and don’t let yourself linger in any wet workout clothes or bathing suits when you wear them, Dr. Dweck advises.
- Don't use fabric softener or dryer sheets on your underwear, Dr. White advises. Instead, opt for a fragrance-free liquid detergent.
- If your vagina is already itchy and it gets worse after condom use, try polyurethane condoms instead of latex, Dr. White says.
- Don't wear your partner's jeans without underwear. Yes, seriously! It can cause discomfort for weeks, Dr. Minkin says.
The bottom line: Vaginal itching can be caused by health issues or completely unrelated to any underlying condition. If your vagina continues to itch after cleansing with a gentle soap and a change of underwear, it's worth checking in with your doc to rule out more serious causes.

Jasmine Gomez is the Commerce Editor at Women’s Health, where she cover the best product recommendations across beauty, health, lifestyle, fitness, and more. When she's not shopping for a living, she enjoys karaoke and dining out more than she cares to admit. Follow her @JazzeGomez.

Ashley Martens is a Wellness Writer based in Chicago, Illinois. With a digital marketing background and her knowledge of general nutrition and a lifelong passion for all things health and wellness, Ashley covers topics that can help people live happier and healthier lives.